Gordie Howe CARES
Who is caring for our caregivers?
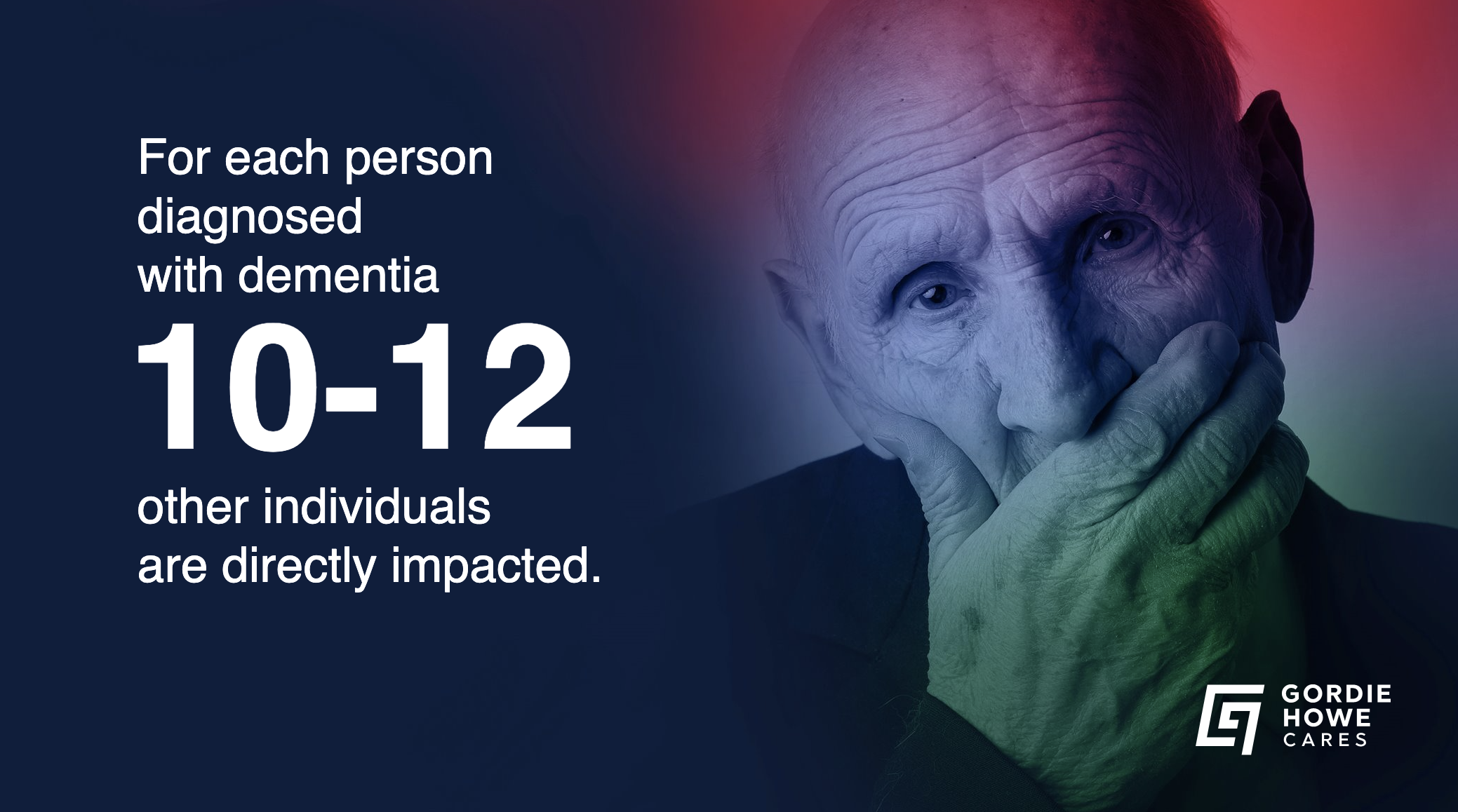
124,000 Canadians were diagnosed with dementia in 2020. For each person diagnosed with dementia, 10-12 other individuals are impacted.
“Informal caregivers … sacrifice their own time, finances and health in order to care for a loved one with dementia.”
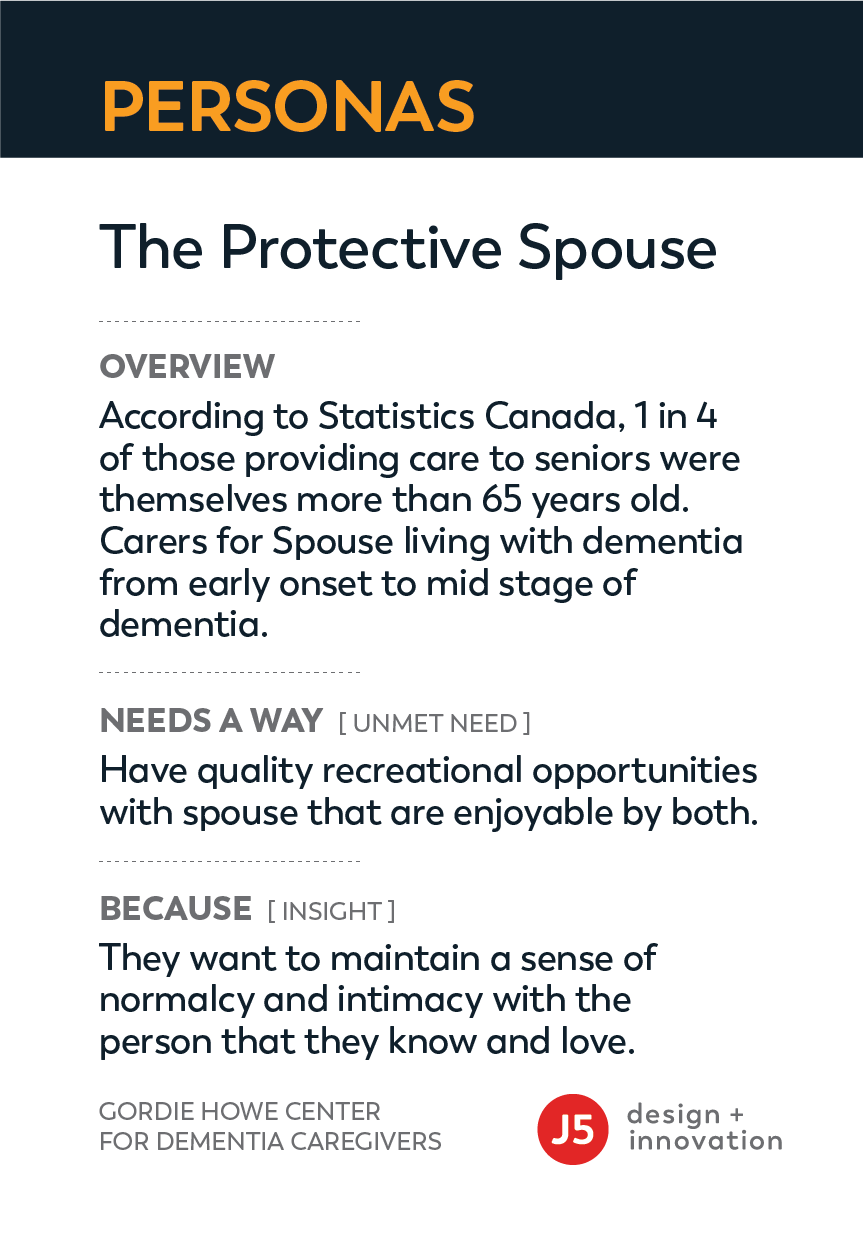
45% of caregivers experience caregiver distress which includes symptoms of anger and depression. 21% feel unable to continue with caring activities. There is an opportunity to better support caregivers so that they can remain healthy, resilient, and have the best quality of life possible. While some readily seek and have access to help, there are many who are hesitant. Stigma of the condition and values around familial duty contribute to many caregivers feeling like they must do it all on their own.
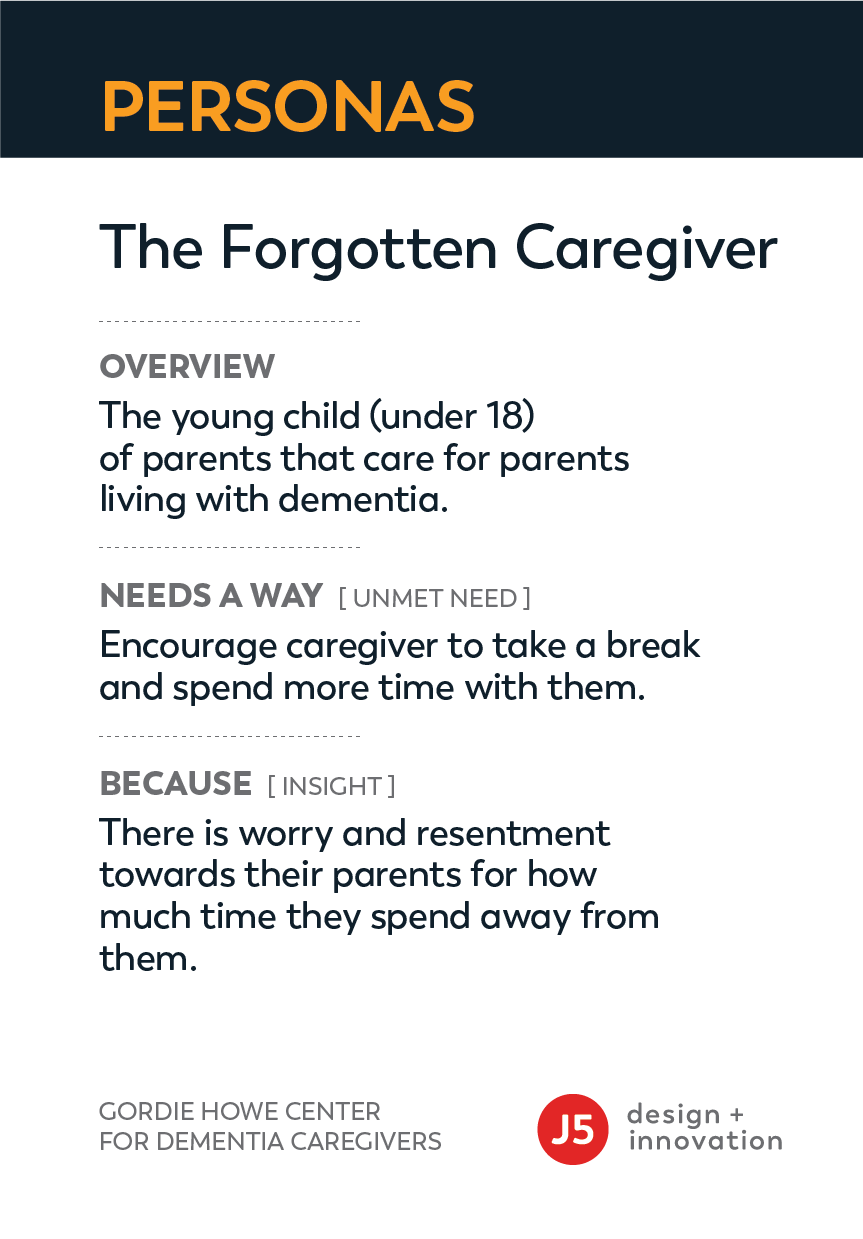
For others, existing services do not match their needs and how they want to be supported. Recognizing and supporting the diversity of caregivers (including across all ages, genders, cultural backgrounds, socio-economic status) necessitates a new and different approach.
Primary Insights
Caregiving feels like climbing a mountain.
After long stretches, steeper elevations and unexpected changes in the terrain, a caregiver’s body and spirit gets tired, it gets harder to continue. There is no turning back, caregivers begin to stumble their way through, second-guessing choices and biting through the pain.
They make it to what they think is the summit, only to realize that there is another peak waiting for them in the distance. When they think of quitting, their heart says “no, people are counting on them to make it through this.” So, they keep going until them or the mountain wins.
Like mountain climbers, caregivers need to take breaks to gather their mental and physical strength to keep pushing forward. If they don’t, the results can be fatal. The bittersweet reality is that many others caregivers have completed the climb and are willing to share their stories and maps to help others find their way.
But how can caregivers find them? That was the question we wanted to answer in this project.
Customer Research
Finding the user.
One of our biggest challenges in this project was finding caregivers to participate in our co-design process. When they are not caring for their loved one with Alzheimers or related Dementias, they are balancing their careers or tending the the needs of their children, spouses and communities.
It’s a full-time job on top of another full-time job. CIHI’s analysis finds that caregivers of seniors with dementia provide an average of 26 hours of care each week. This is substantially higher than the 17 hours provided by caregivers of those without dementia.
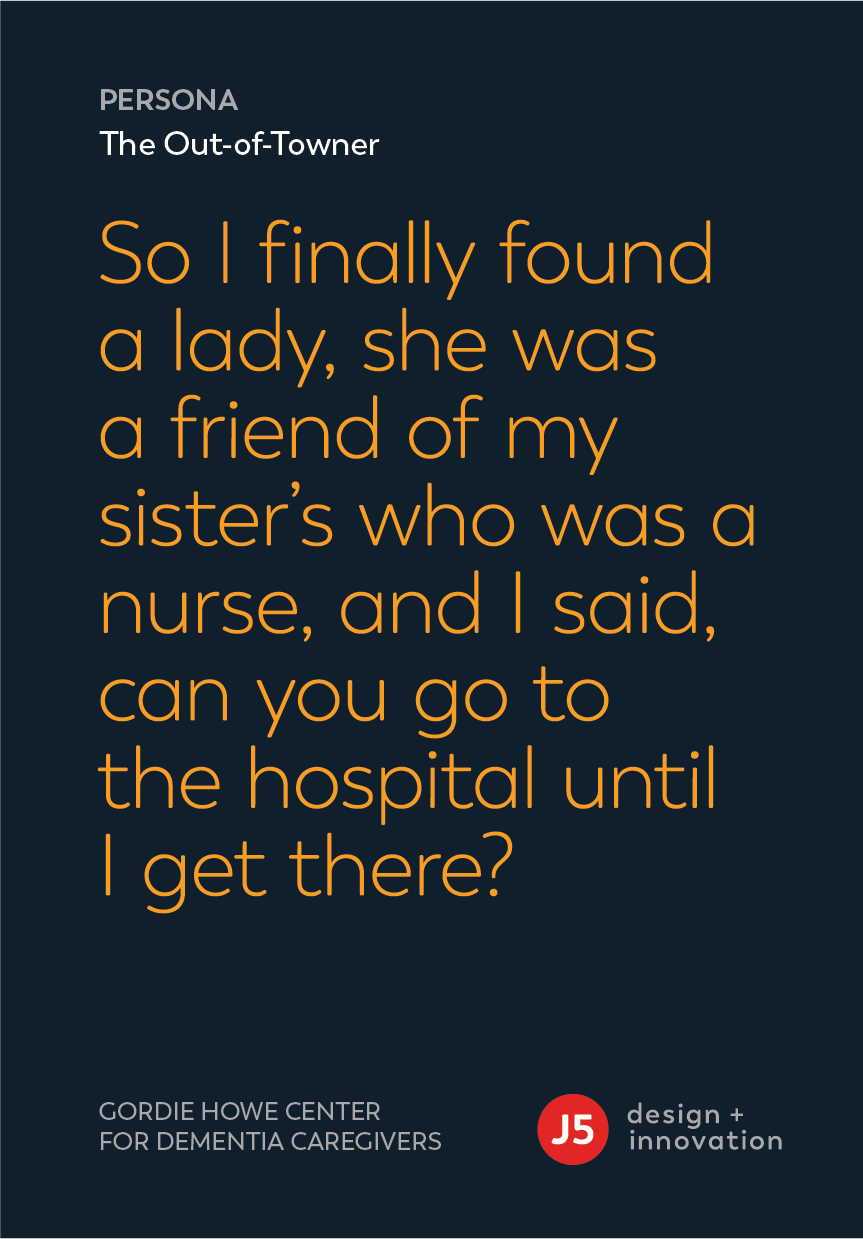
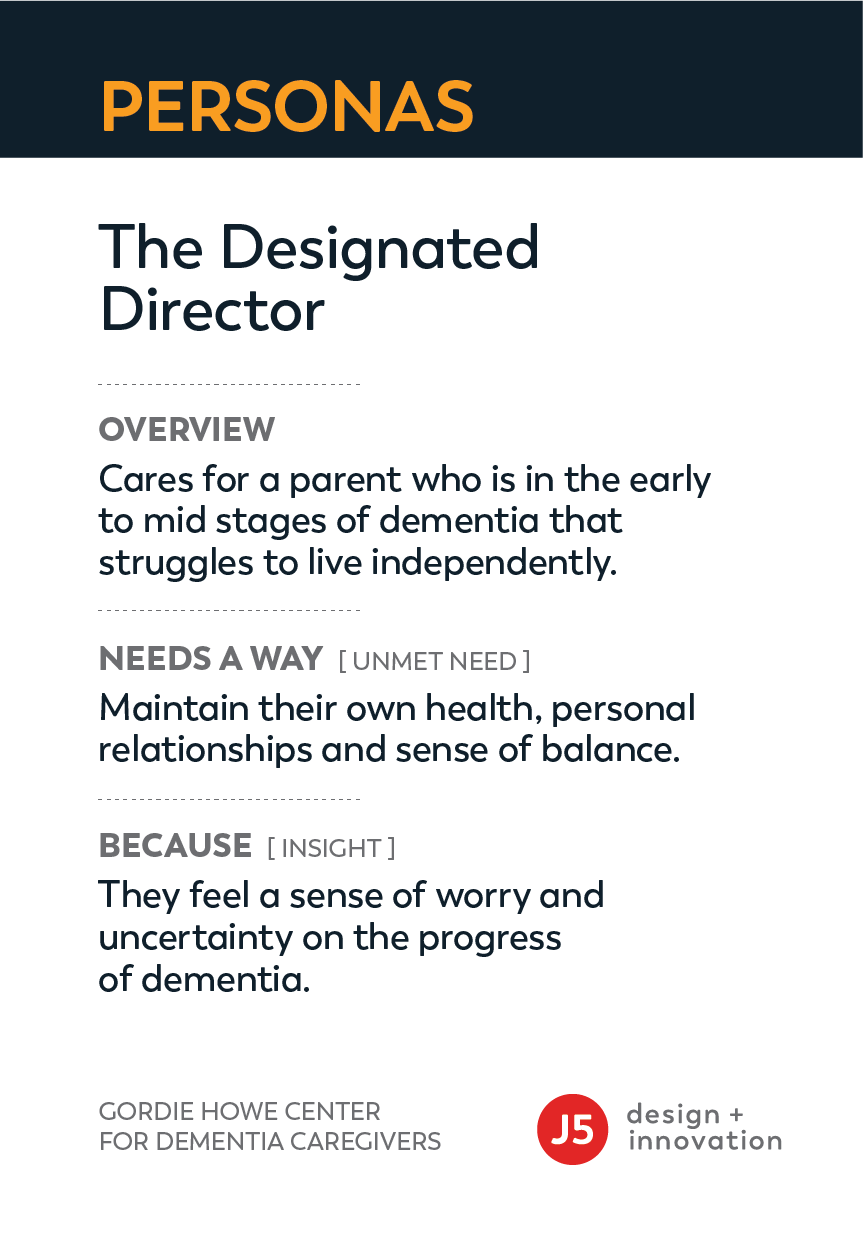
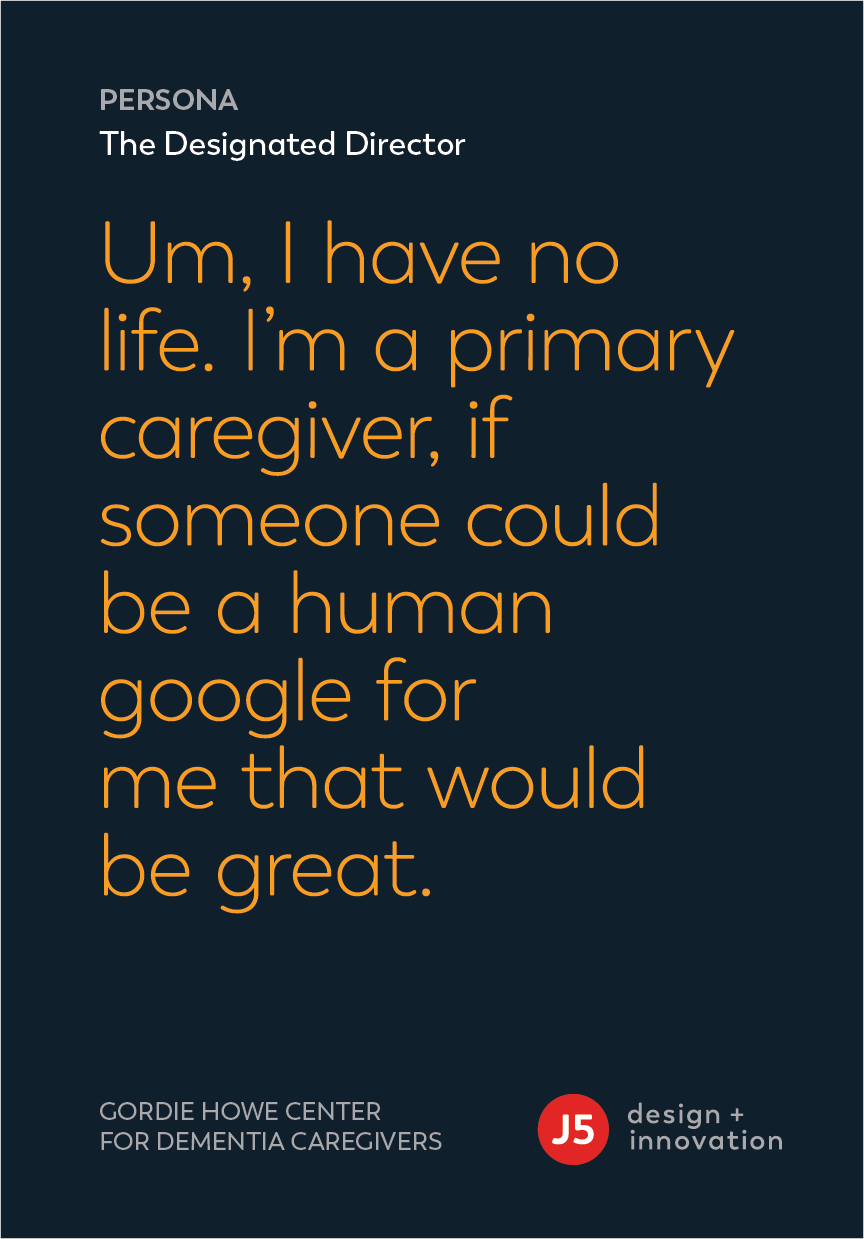
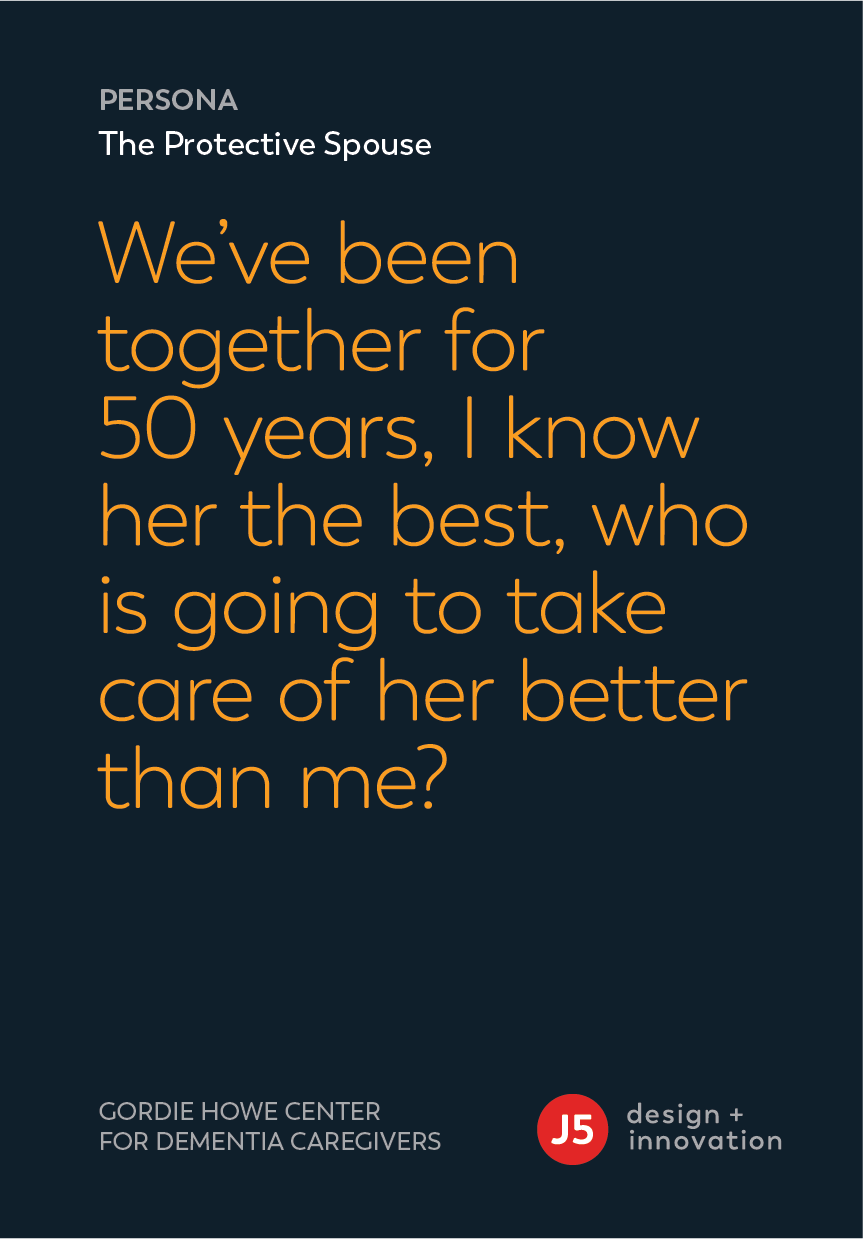
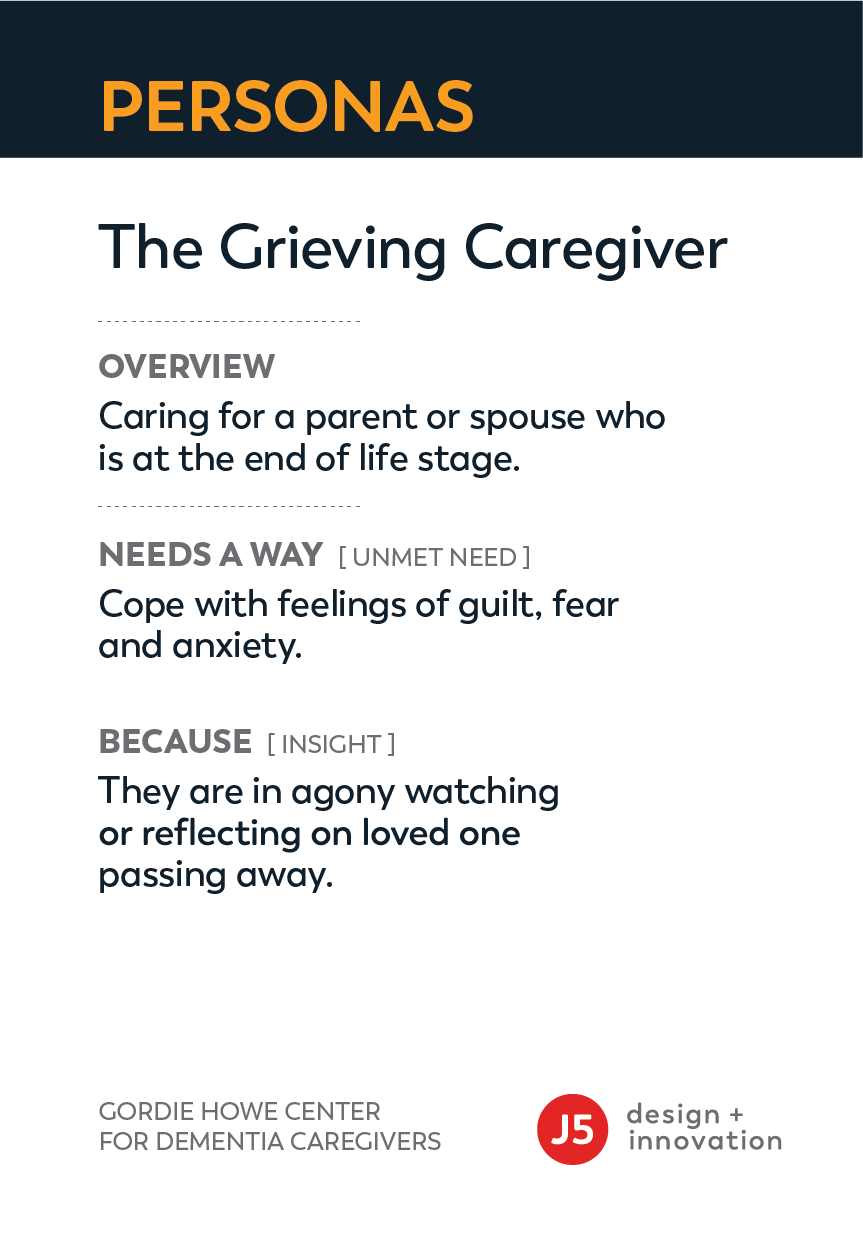
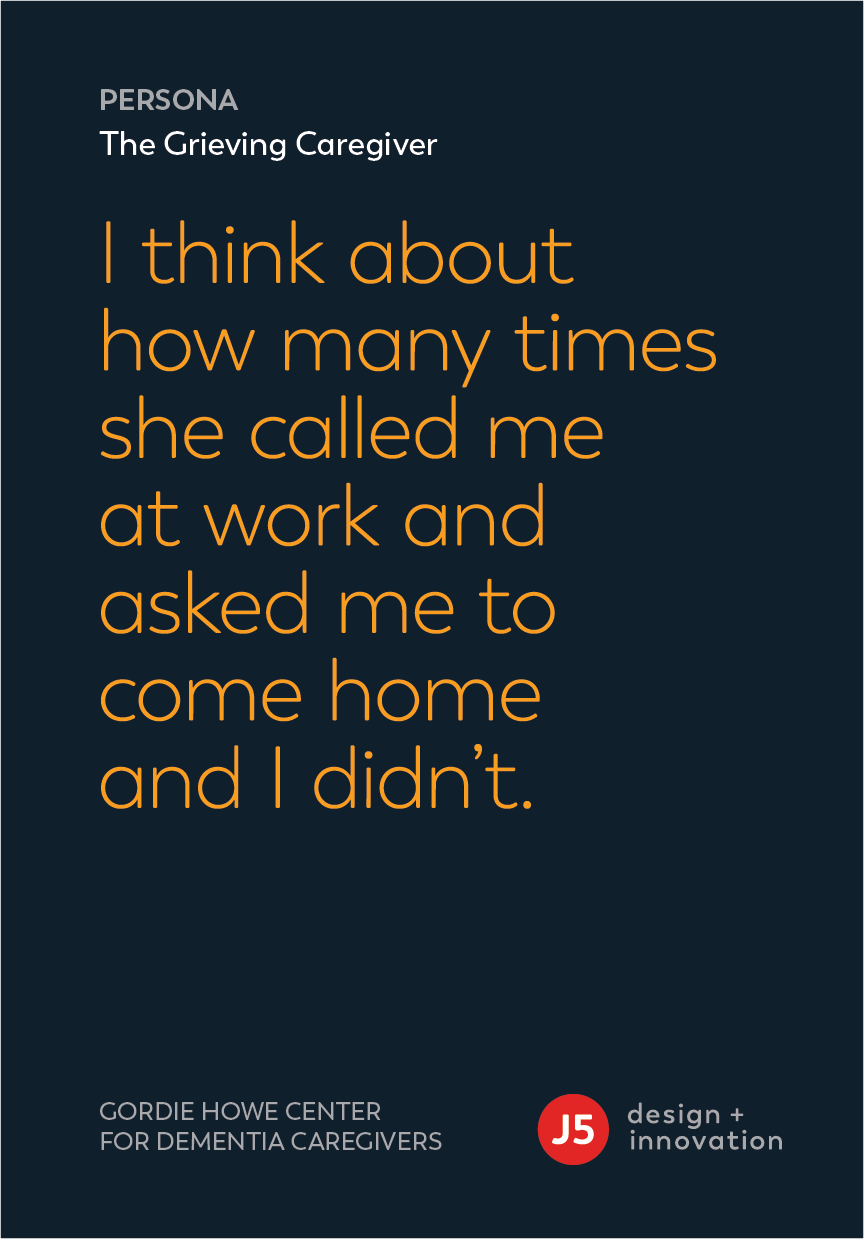
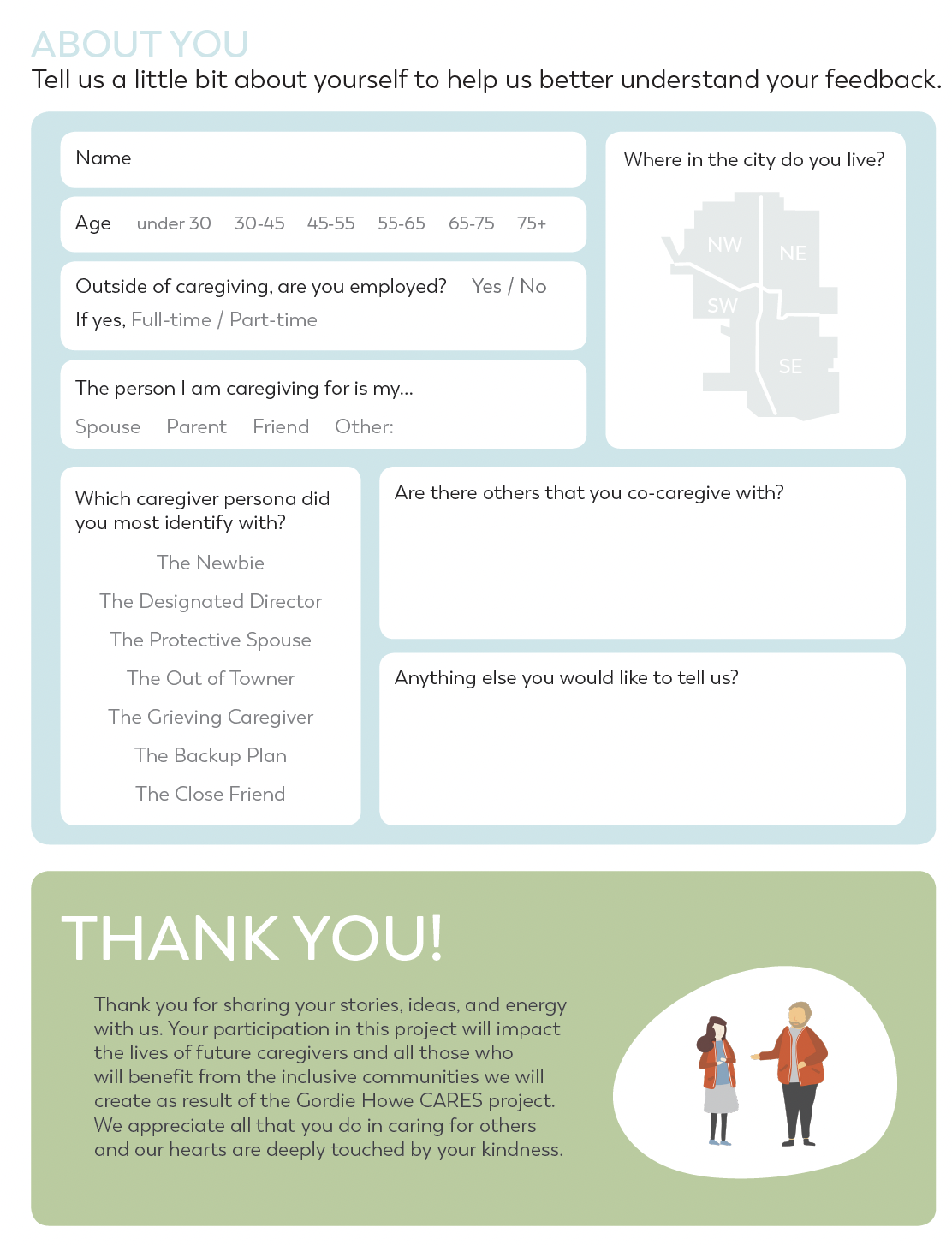
Our project started by meeting with over 50 caregivers in coffee shops, across kitchen tables, and over the phone and listening to their stories of trauma, frustration, joy, and resilience. We captured what we heard in our conversations and began building personas including: “The Newbie” caregiver that need help persuading a parent to get a diagnosis or “The Out of Towner” who would agonize about being faraway with little visibility into what is happening.
We then layered these personas (nine of them) with data around technology, lifestyle, and spending habits and created more holistic visuals of their respective caregiver journeys.
Testing Assumptions
Rapid prototyping.
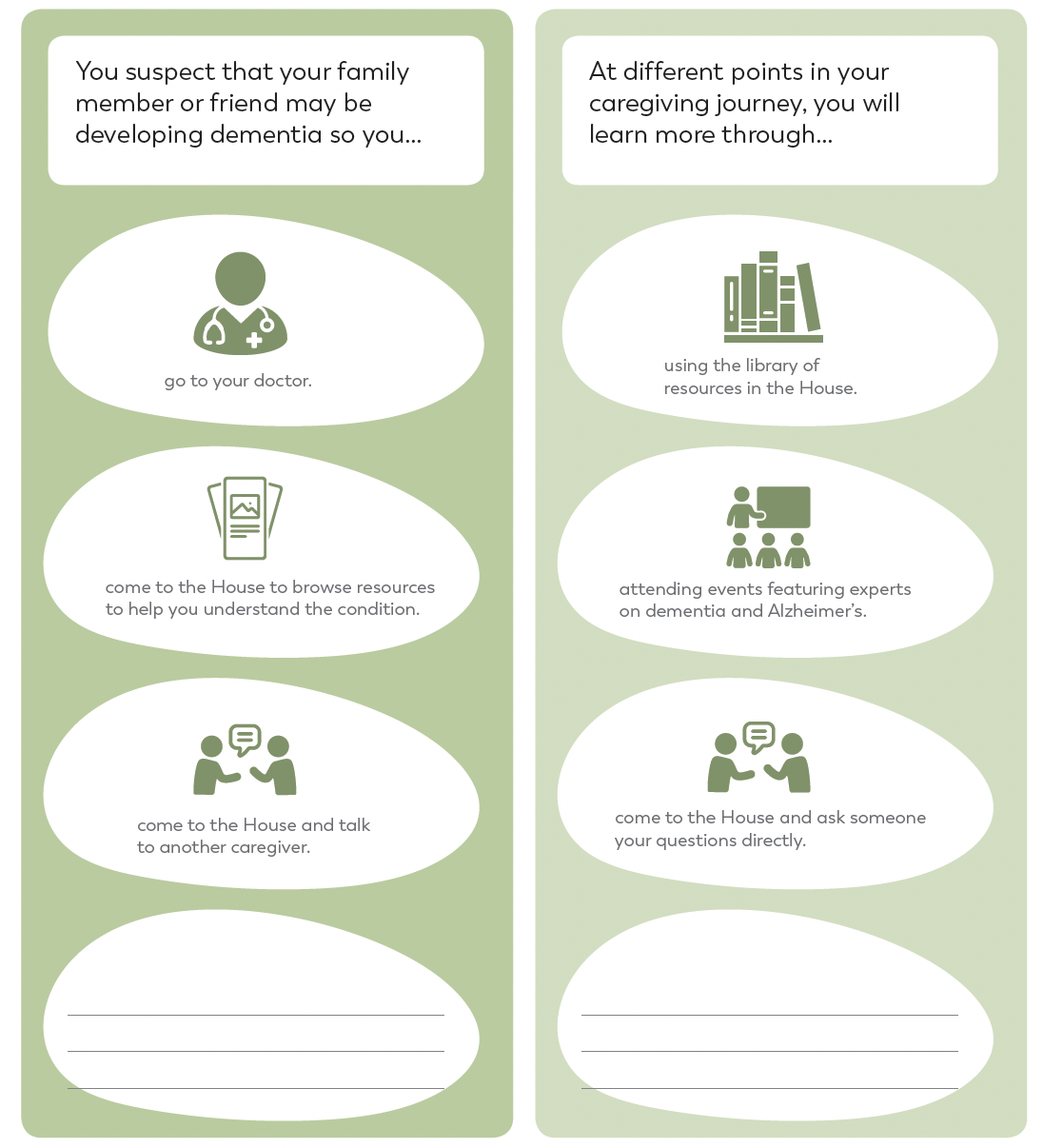
From our discussion with caregivers, we identified that there are periods of high stress surrounding transitions related to changes in the health of the person they are caring for and the additional caring responsibilities that result.
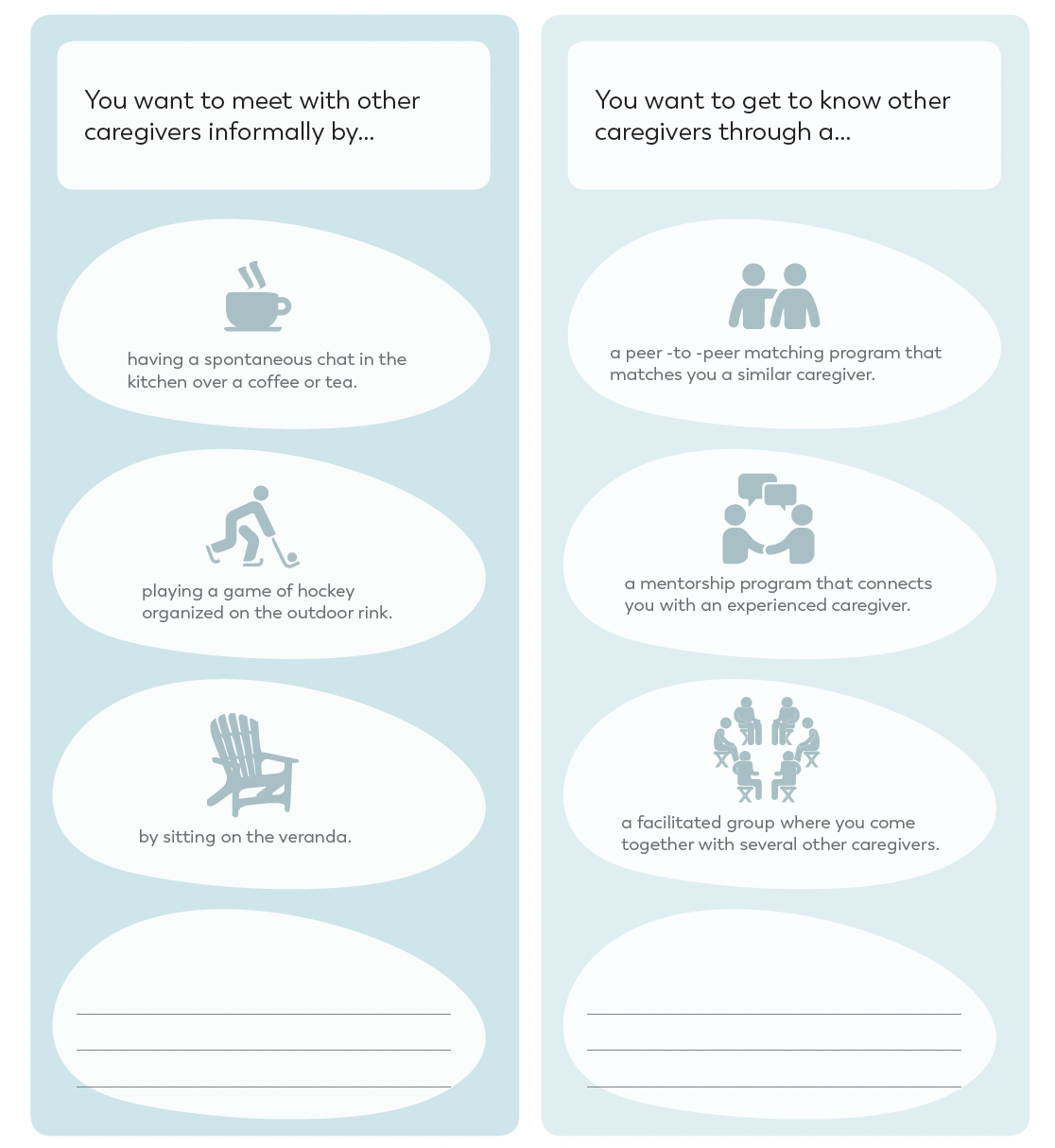
Digging deeper, we created videos, choose your own adventure books, mock websites, sketches, and storyboards to test potential concepts with caregivers in co-design sessions all over Calgary. We probed them about what services were priorities and the kinds of experiences that they love to engage in.
Our big takeaways:
By focusing on engaging caregivers during the low stress periods and guiding them to prepare for upcoming transitions, we can reduce stress levels and prevent burnout.
Caregivers respond to environments where they can share stories, have meaningful conversations and validate their own feelings.
Caregivers are hard to find, particularly those in the early stage
Caregivers are not aware of their (potential) care team for their loved one
Supporting marginalized or rationalized communities requires a careful approach and partners with experts in this space
Solution
Digital Solution.
Our research and customer engagement led us to a solution of a digital solution where caregivers could learn about best practices at their own pace from curated and credible materials, and receive immediate guidance from online coaches and peers.
By creating a self-service tool for caregivers that makes them feel safe and appreciated, Gordie Howe CARES wants to guide them through the inevitable ups and downs of their own journeys, help them to push through adversity and reach the summit with confidence, pride, and support.
Learn more at https://www.gordiehowecares.com/


